25 Surprising Facts About Rheumatoid Arthritis


25 Facts About Rheumatoid Arthritis (RA) Everyone Should Know
Rheumatoid arthritis is an illness that’s widely misunderstood. I believe this is partly due to the fact that many confuse it with osteoarthritis (OA). This mix-up leads people to believe rheumatoid arthritis is caused by aging.
Rheumatoid arthritis (RA) is in no way “normal” aging and shouldn’t ever occur at any point in a healthy person’s life!
Rheumatoid arthritis is an autoimmune disease – meaning the body’s immune system is attacking itself – in the case of RA the immune system attacks a person’s joints.
Almost 1.5 million Americans have rheumatoid arthritis and it’s on the rise. Unfortunately, modern medicine doesn’t have much to offer for reversal of this terrible condition. However, functional medicine and full body integrative and holistic approaches have resulted in full recoveries and promising outcomes.
I am a perfect example of this. I was diagnosed with Rheumatoid Arthritis (I was also given many other additional diagnoses – another blog on this later) more than a decade ago. When modern medicine had no answers for me other than prescribing toxic immunosuppressive drugs and steroids, I voluntarily chose not to use those. As a practicing Internal medicine doctor who had a special interest in Rheumatology, I knew all too well, the terrible side effects and long term health consequences of these drugs. I was determined to find other answers!
Against conventional wisdom, I decided to be my own guinea pig and looked for other safer but effective alternatives. I researched and studied the fields of nutrition, and Integrative, Holistic, and Functional Medicine. I trained and became board certified in these, using all that I learnt, first on myself. It was trial and error at that point for me but I eventually healed myself from this crippling disease and from all other diagnoses that conventional medicine had given to my wide range of chronic symptoms!
My health completely recovered, and I no longer carry the clinical or lab diagnosis of RA, nor do I suffer from the pain or the disabling fatigue which is characteristic of this disease. In fact, I feel more energetic and vibrant than I did even in my 20s. I now use the same healing modalities and step-wise approach that worked for me, on my patients to help them in their recovery process.
As with everything else in life, we are all individuals with unique and varied characteristics, so no one size of treatment can fit all. Everyone with RA will have different root cause(s). I help my patients and clients find their particular root causes and then use a very personalized treatment approach that is right for their body.
In an effort to clear the confusion and misunderstanding surrounding rheumatoid arthritis, I’ve compiled 25 facts about rheumatoid arthritis that everyone should know. RA is a condition that can strike any person at any age – and it’s best to know these important facts.
1. Rheumatoid arthritis (RA) is very different from osteoarthritis (OA)
RA is an autoimmune disease while osteoarthritis is caused by erosion of the cartilage and bones due to aging, overuse or obesity. Because these conditions are completely different, so are their treatments and it is important not to confuse the two.
2. Rheumatoid arthritis is not ‘normal’ wear and tear of the joints
Rheumatoid arthritis occurs when the body’s immune system attacks its joints. This attack results in painful inflammation of the hands, feet, knees and other joints. RA can also impact other tissues in the body such as the heart, lungs, mouth, and eyes.
3. Rheumatoid arthritis is more prevalent now than ever before
Many articles on RA like to cite the fact that there’s very little evidence RA existed before the 1500’s, however that fact remains uncertain. What we do know, is RA is more prevalent now than ever before and it’s incidence is on the rise. This fact leads many to believe it is a disease caused primarily by environmental factors such as diet and toxins.
4. Children can develop Rheumatoid Arthritis

It’s possible for children to develop RA -known as Juvenile Rheumatoid Arthritis (JRA) – because it’s an autoimmune condition, not caused by aging. In fact, children as young as five years old can develop RA, which is a deeply troubling to witness.
5. Rheumatoid Arthritis is usually worst in the hands and feet

Though RA can impact any joint and many tissues in the body, it’s most common in the hands and feet. RA attacks the synovial lining between the bones of a joint, causing it to become inflamed, and ultimately damaging the tissue. Over time, RA can cause deformity to the affected joint.
6. Women are three times more likely to develop RA

For reasons that are not fully understood, women are three times more likely to develop RA than men. It is thought that hormones may play a role. Also, the prevalence of RA among women is on the rise.
7. Geography influences RA risk

RA is more common in people who live further from the equator, which suggests that adequate sunshine could help reduce RA risk, which leads me to my next point…
8. Vitamin D reduces risk of developing RA

Sufficient vitamin D significantly reduces your risk of developing RA and sunshine is your best source of vitamin D. Vitamin D has been linked to a reduced risk for nearly all autoimmune disease, so it’s a good idea to daily get about 20 minutes of sunshine, before applying sunscreen (without burning of course). If you have the ability to test your vitamin D levels, please do so and take supplemental Vitamin D under supervision. In my practice I use different strengths of Vitamin D based on my patient’s levels.
9. Exercise is usually recommended in RA

Surprising to some, physical therapy has been shown to improve symptoms of RA. Decades ago, doctors believed exercise would put unnecessary stress on joints and recommended against it. This belief is not true and proper exercise with rheumatoid arthritis is now encouraged.
10. Diet is a vital part of treatment of Rheumatoid Arthritis

Anti-inflammatory diets low in gluten, sugar, processed and fried foods are an integral part of the functional medicine approach to RA. I would recommend working with a Functional medicine doctor and getting detailed food, nutritional and gut assessment so your individual causes for RA can be specifically dealt with.
11. Chronic inflammation is a major component of RA

Rheumatoid arthritis goes hand-in-hand with chronic inflammation. This means you can do yourself a world of good by incorporating anti-inflammatory practices in your life through diet, by reducing the burden of toxins in your body, and by targeted supplementation. The fire needs to be quenched!
12. Muscle atrophy is a concern in RA

Due to the lack of appetite that accompanies RA, coupled with the misguided but common belief that exercise will make RA worse, many people in the past suffered from muscle atrophy. These issues led to the nickname “wasting disease” because those with RA were often rail-thin and “wasting away.” A typical complaint is difficulty opening jars. Adding a daily protein drink or two to your nutritional supplementation can most certainly help replenish muscle strength. . My favorite protein powders are ones which also help gentle detox of the liver and the body.
13. Loss of appetite is common in RA

Due to inflammation of the gut, many with RA experience a strong loss of appetite, which contributes to weakness and muscle atrophy. The best way to fight this is through healing the gut and reducing inflammation.
14. A genetic risk factor called a “shared epitope” in RA

A shared epitope (SE) is a genetic variant that increases the likelihood of developing RA when present, in fact some studies suggest that SE is the single most significant genetic risk factor for RA. Though there’s a genetic predisposition for RA, most believe risk is more associated with environmental factors. Remember, genes are loaded guns but environmental exposures hold the trigger!
15. Heart disease is a problem for RA patients

Having RA significantly increases your risk for developing cardiovascular disease and having a heart attack. This is likely due to the characteristic systemic inflammation present in both conditions.
16. Diabetes risk is higher in RA patients
RA increases the risk of many illnesses, including diabetes, though this could also be caused by the conventional RA treatments, which quite often include intermittent or chronic steroid use. Steroids increase the risk for diabetes. Opting for a functional medicine approach to rheumatoid arthritis could reduce this risk.
17. Fibromyalgia risk is higher in RA patients

There is an increased risk for developing fibromyalgia in patients with RA. Suffering from a combination of these two illnesses can lead to chronic pain, severe depression, fatigue, as well as memory and cognitive issues.
18. Lung disease is a common complication in RA patients
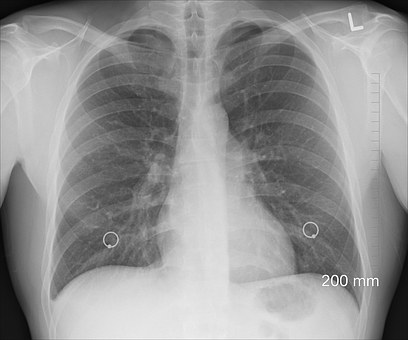
Interstitial lung disease, a serious lung disease can be a frequent complication of RA when the disease activity is not properly controlled, in fact after joints, lungs are the second most common organ to be affected by this disease. Serious respiratory conditions, infections and pneumonia can also occur due to conventional treatments which suppress the immune function; or due to lifestyle habits such as smoking. Any symptom of shortness of breath should be properly investigated.
19. Pregnancy can temporarily improve RA symptoms

Pregnancy often improves symptoms of many diseases, including RA. I believe this is because of the elevated anti-inflammatory elements present in the body during pregnancy, such as the DAO enzyme. However, after a person with RA gives birth, they could experience a flare-up and should plan with their doctor accordingly. Postpartum follow up of RA and for that matter any autoimmune condition is crucial.
20. Giving birth reduces risk for developing RA

Though the reason behind this is not fully understood, research has shown that giving birth reduces a woman’s overall risk of developing RA compared with someone who has never given birth.
21. Smoking increases RA risk and worsens symptoms overall

Smoking cigarettes increases a person’s risk for developing RA. Additionally, smoking cigarettes is a serious trigger for a flare of RA and can worsen symptoms overall.
22. It’s unclear whether alcohol is bad or good for RA

Studies have been published suggesting some alcohol is both good and bad for people affected by RA. It’s my recommendation that you consume as little as possible because alcohol makes it difficult for your body to work on ridding itself of toxins in your everyday life that could be contributing to your RA.
23. Pollution increases Rheumatoid Arthritis risk

Pollution is known to cause inflammation in the body, so it’s no surprise that researchers found women who lived within a third of a mile of a major highway had higher prevalence of systemic inflammation and RA.
24. Psychological stress can have a role in RA
Stress is one of the factors that may not only cause and but also exacerbate the progression of chronic inflammatory diseases such as RA. Relapses are common under conditions of emotional stress. Treatments based on mindful awareness and acceptance therapies lead to reductions in daily pain-related sense of doom and disability, fatigue, as well as stress-related anxiety in RA patients. A holistic mind-body approach is paramount along with other Functional medicine treatments for RA.
25. Functional medicine solutions are promising in RA

Steroids and NSAIDs (some of the conventional treatments for RA) are not a good long term treatment plan. Not only do they not offer long term solutions, they are harmful to the gut and the immune system! They work against the very systems that need healing.
Instead try a functional medicine approach to RA treatment with your Functional Medicine doctor, which includes:
- Anti-inflammatory diet – Free of gluten, sugar, fried, and processed foods.
- Reducing toxin burden – Cleaning up your household products and cosmetics is a good start. Only use ‘clean’ personal care products without hormone dysrupting chemicals.
- Healing a leaky gut – You’ll need to repair your gut lining to help your immune system regain strength. I use a special gut support powder, digestive enzymes and probiotics to balance the gastrointestinal tract function.
- Check for bacterial and yeast overgrowth – work with your Functional Medicine doctor to diagnose and treat these.
- Check for mycotoxins – Your doctor can also test you for mycotoxins which come from mold. Read my article here on mold clean-up..
- Heal any infections – Infections with viruses, yeast, parasites and bacteria can mess with your gut health. Among other infectious causes, Epstein-Barr virus is thought to be a trigger of RA.
- Supplementation – Omega-3s, probiotics, vitamin D3, bioavailable forms of curcumin are some of the simple ways to fight the chronic inflammation caused by RA.
Rheumatoid arthritis is a debilitating disease but there are better solutions beyond prescriptions. Reach out to your functional medicine doctor if you or someone you love suffers from rheumatoid arthritis.
Please share this article to help dispel common myths surrounding rheumatoid arthritis.
Please also share how you manage your disease and help others learn from your experiences.
Resources:
https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024678/
http://www.arthritis.org/about-arthritis/types/rheumatoid-arthritis/what-is-rheumatoid-arthritis.php
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119866/
https://www.niams.nih.gov/health_info/Juv_Arthritis/default.asp
https://www.rheumatoidarthritis.org/ra/
https://www.ncbi.nlm.nih.gov/pubmed/14730601
https://www.ncbi.nlm.nih.gov/pubmed/28808949
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3766928/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2921962/
https://www.ncbi.nlm.nih.gov/pubmed/24736263
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3890244/
https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284707/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2717131/
https://www.ncbi.nlm.nih.gov/pubmed/24850878
https://www.ncbi.nlm.nih.gov/pubmed/28638686
https://www.ncbi.nlm.nih.gov/pubmed/25365778
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1526553/
Dr. Manisha Ghei October 3rd, 2017
Posted In: Blog Post, Functional Medicine, Functional Nutrition, Integrative Medicine, Rheumatoid Arthritis, Uncategorized
Tags: Autoimmune, Autoimmune disease, Autoimmune MD, Autoimmunity, Chronic fatigue syndrome, fibromyalgia, functional medicine, heart health, Inflammation, Joint, nutrition, OA, Osteoarthritis, RA, Rheumatoid Arthritis, supplements, women
8 Essential facts about Omegas -Essential Fatty Acids (EFAs)

Essential Fatty Acids (EFAs) – Essential to Brain Health
I’m often asked what are the few nutrients I think are absolutely imperative and essential for good health especially in this modern world. One of the top nutrients in my list is Omega Essential Fatty Acids. Every patient who comes into my practice gets their Omega 3 levels and the ratio of Omega 3s to other omegas, like 6s, 9s etc tested and an appropriate individualized diet and supplementation (if required) plan created for them.
Decades of study and countless books have gone into exploring Omega-3 and the role it plays in our physical and mental health.
Here are 8 Essential Facts about this ESSENTIAL substance.
1. Omega-3 is called “essential” because it’s necessary for our health, but we cannot make it on our own.
2. One essential Omega-3 fatty acid is a substance called α-linolenic acid (ALA). Our body can use ALA to make two other essential fatty acids: DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid). However, we don’t make enough to meet daily needs for optimal health and the conversion of ALA to DHA and EPA is not efficient enough in most humans.
If you are deficient in Vitamin Bs of various kinds, Vitamin C, minerals like Magnesium and zinc you will not optimally convert ALA into DHA and EPA.
Have your physician test you for optimal levels of these nutrients and adjust your dietary plan and your supplement schedule to optimize the levels of these key supportive nutrients.
You may benefit from supplementation with:
- a B complex containing activated forms of B vitamins,
- a highly absorbable and bio-available form of magnesium (that does not cause diarrhea)
- a highly absorbable and bio-available form of zinc
- a highly absorbable and bio-available form of Vitamin C with bioflavanoids
- A comprehensive Multivitamin and Multimineral supplement. If you’re a menstruating woman, you may wish to take the version that contains iron as well.

3. Omega-3 is critical for preventing symptoms of chronic illness, such as inflammation, chronic fatigue, joint and muscle pain and poor elimination of toxins.
4. The brain thrives on Omega-3. Without enough, we can experience learning problems, memory issues, brain fog, ADHD symptoms and other neurological symptoms. Proper levels help protect us from Alzheimer’s Disease. Balanced omega fatty acids are crucial in cardiovascular health and healthy blood pressure maintenance and insulin and blood sugar balance.
5. Food is a great source of Omega-3. Consider fatty fish like salmon, tuna, halibut, krill, flaxseed, walnuts and chia seeds (the latter 3 however give us ALA which needs to be converted to DHA & EPA).
6. It’s difficult to get sufficient amounts from food alone. Most Americans consume a daily average of 130 mg EPA + DHA – way below the recommended 1000-2000 mg. Consider adding a supplement to your diet. The Omega 3 supplement my family and I use, and I recommend to patients in my practice is International Fish Oil Standards (IFOS) five-star certified, which assures the highest level of purity, stability, and potency in fish oils. Each dose of this concentrated fish oil provides a whopping 900 mg of EPA and DHA in one softgel. Always check the the EPA and DHA content at the back of your bottle, as many times manufacturers will list a certain mg of fish oil on the front label of the fish oil bottle and it does not provide the accurate amounts of EPA and DHA that each serving has. This can mislead the buyer.
7. Acquiring Omega-3 must be done in a focused fashion, with attention paid to the balance between Omega-3 and Omega-6 (a group of fatty acids linked to increased inflammation). An imbalance can adversely impact well being and brain health.
8. Not all Omega 6s are bad! One known as DGLA (Dihomo-gamma-Linoleic Acid) is an antiinflammatory Omega 6 fatty acid. Other ones known as LA (Linoleic Acid) and AA (Arachindonic Acid) can be inflammatory in high amounts or when not in balanced amounts compared with DGLA. 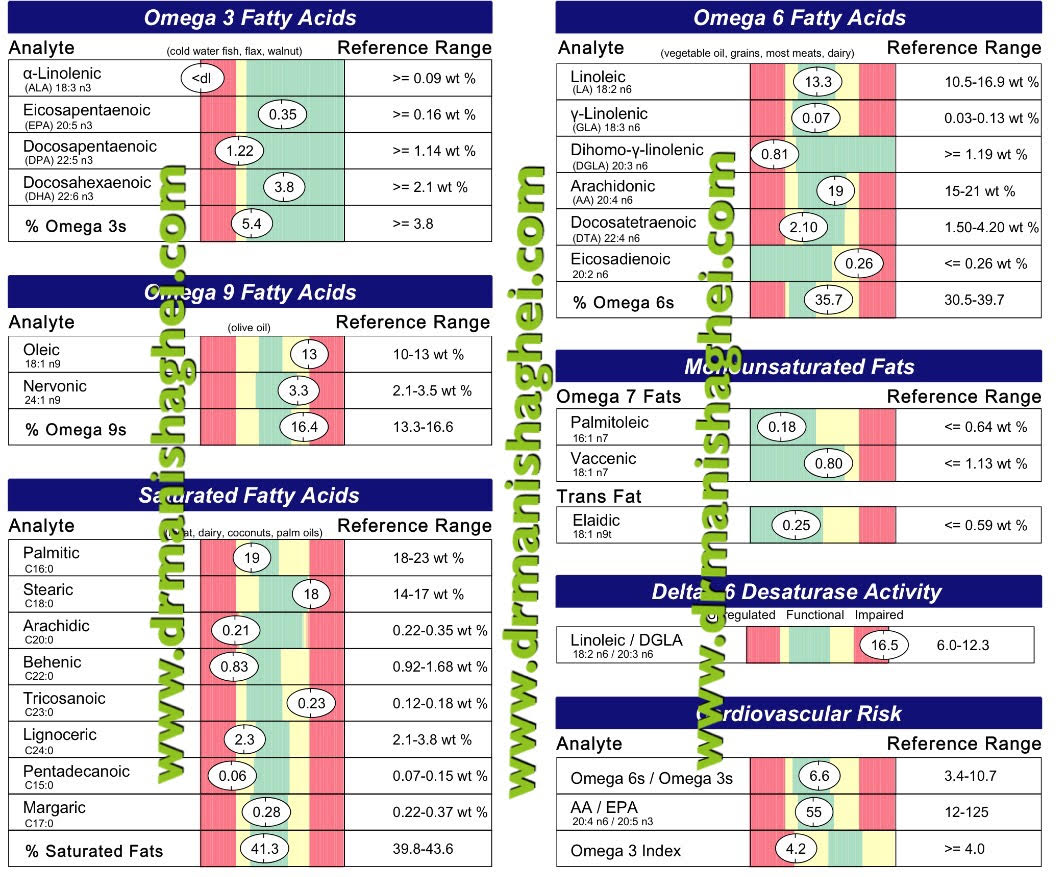
In my testing I look at individual levels of these key Omega 3 and 6 Fatty Acids but also the ratio of Linoleic to DGLA as seen in the image above. A simple blood test can give me all of the above information.
Consult your Functional Medicine and / or Integrative Holistic Medicine physician to assess your intake, test your levels, and explore ways to help you protect your health and cognitive function with essential Omegas.
References:
-
University of Maryland CAM Database Online. “Omega-3 Fatty Acids” Accessed 7 Nov 2016: http://umm.edu/health/medical/altmed/supplement/omega3-fatty-acids
-
Assisi A., Banzi R., Buonocore C., et al. “Fish oil and mental health: the role of n-3 long-chain polyunsaturated fatty acids in cognitive development and neurological disorders.” Int Clin Psychopharmacol. 2006 Nov;21(6):319-36. Accessed 7 Nov 2016: https://www.ncbi.nlm.nih.gov/pubmed/17012979
-
Ricardo U., Dangour, A.D. “Nutrition in Brain Development and Aging: Role of Essential Fatty Acids” Nutrition Reviews (May 2006)64 (suppl 2) S24-S33; DOI: 10.1111/j.1753-4887.2006.tb00242.x http://nutritionreviews.oxfordjournals.org/content/64/suppl_2/S24
-
Bourre, J.M. “Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain. Part 2: macronutrients”. J Nutr Health Aging. 2006 Sep;10(5):386-99. Accessed 7 Nov 2016: http://www.bourre.fr/pdf/publications_scientifiques/260.pdf
-
NutritionData.com. Foods Highest in Total Omega-3 Fatty Acids. Accessed 7 Nov 2016. http://nutritiondata.self.com/foods-012140000000000000000.html?maxCount=20
-
Freund-Levi Y, Eriksdotter-Jonhagen M, Cederholm T, et al. “Omega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: a randomized double-blind trial.” Arch Neurol. 2006 Oct;63(10):1402-8. Accessed 7 Nov 2016: http://www.utdallas.edu/~tres/papers/freund-levi.2006.pdf
The information offered by this blog is presented for educational purposes. Nothing contained within should be construed as nor is intended to be used for medical diagnosis or treatment. This information should not be used in place of the advice of your physician or other qualified health care provider. Always consult with your physician or other qualified health care provider before embarking on a new treatment, diet or fitness program. You should never disregard medical advice or delay in seeking it because of any information contained within this blog. © Praana Integrative Medicine & Holistic Health Center, LLC. All rights reserved
Dr. Manisha Ghei April 16th, 2017
Posted In: Blog Post, Food, Functional Medicine, Integrative Medicine
Tags: ADHD, allergies, antioxidant, arthritis, asthma, blood pressure, cancer, cholesterol, Chronic fatigue syndrome, dementia, Diabetes Mellitus, fibromyalgia, functional medicine, healthy heart, heart healthy foods, Inflammation, Insulin, Memory, nutrition, Omega 3, vascular health








