Essential Fatty Acids (EFAs) – Essential to Brain Health
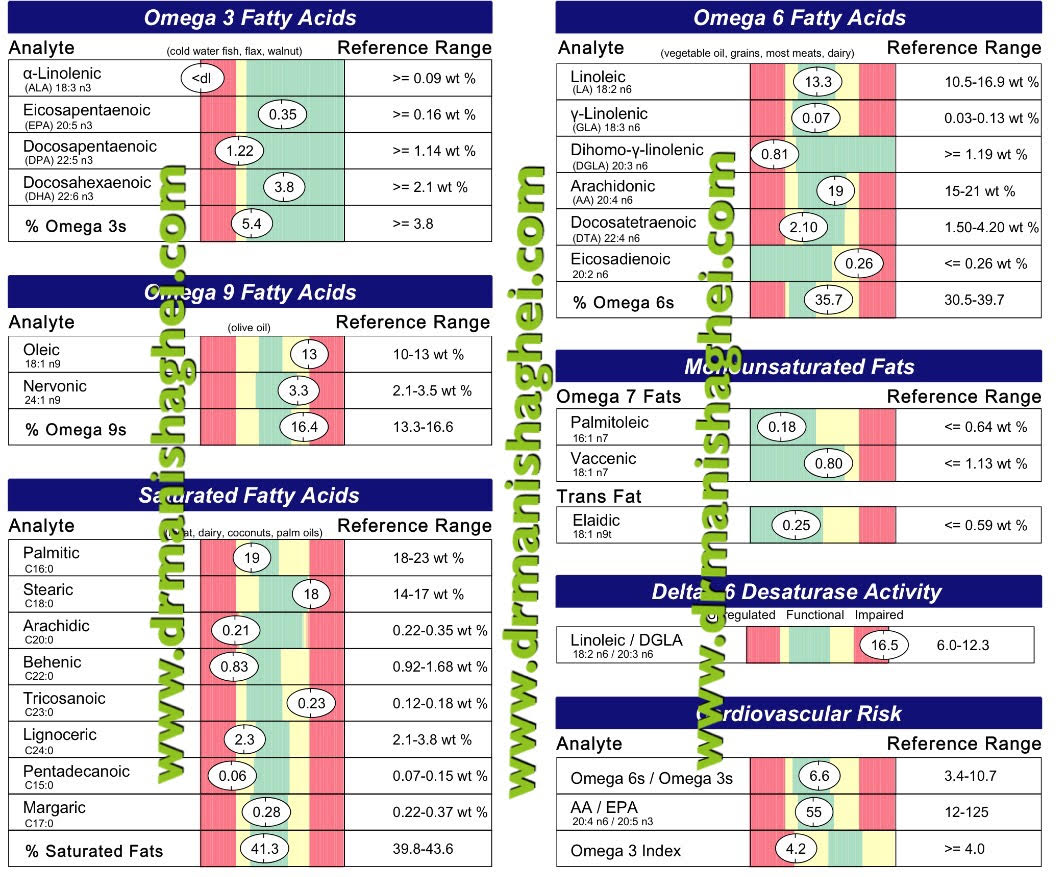
I’m often asked what are the few nutrients I think are absolutely imperative and essential for good health especially in this modern world. One of the top nutrients in my list is Omega Essential Fatty Acids. Every patient who comes into my practice gets their Omega 3 levels and the ratio of Omega 3s to other omegas, like 6s, 9s etc tested and an appropriate individualized diet and supplementation (if required) plan created for them.
Decades of study and countless books have gone into exploring Omega-3 and the role it plays in our physical and mental health.
Here are 8 Essential Facts about this ESSENTIAL substance.
1. Omega-3 is called “essential” because it’s necessary for our health, but we cannot make it on our own.
2. One essential Omega-3 fatty acid is a substance called α-linolenic acid (ALA). Our body can use ALA to make two other essential fatty acids: DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid). However, we don’t make enough to meet daily needs for optimal health and the conversion of ALA to DHA and EPA is not efficient enough in most humans.
If you are deficient in Vitamin Bs of various kinds, Vitamin C, minerals like Magnesium and zinc you will not optimally convert ALA into DHA and EPA.
Have your physician test you for optimal levels of these nutrients and adjust your dietary plan and your supplement schedule to optimize the levels of these key supportive nutrients.
You may benefit from supplementation with:
3. Omega-3 is critical for preventing symptoms of chronic illness, such as inflammation, chronic fatigue, joint and muscle pain and poor elimination of toxins.
4. The brain thrives on Omega-3. Without enough, we can experience learning problems, memory issues, brain fog, ADHD symptoms and other neurological symptoms. Proper levels help protect us from Alzheimer’s Disease. Balanced omega fatty acids are crucial in cardiovascular health and healthy blood pressure maintenance and insulin and blood sugar balance.
5. Food is a great source of Omega-3. Consider fatty fish like salmon, tuna, halibut, krill, flaxseed, walnuts and chia seeds (the latter 3 however give us ALA which needs to be converted to DHA & EPA).
6. It’s difficult to get sufficient amounts from food alone. Most Americans consume a daily average of 130 mg EPA + DHA – way below the recommended 1000-2000 mg. Consider adding a supplement to your diet. The Omega 3 supplement my family and I use, and I recommend to patients in my practice is International Fish Oil Standards (IFOS) five-star certified, which assures the highest level of purity, stability, and potency in fish oils. Each dose of this concentrated fish oil provides a whopping 900 mg of EPA and DHA in one softgel. Always check the the EPA and DHA content at the back of your bottle, as many times manufacturers will list a certain mg of fish oil on the front label of the fish oil bottle and it does not provide the accurate amounts of EPA and DHA that each serving has. This can mislead the buyer.
7. Acquiring Omega-3 must be done in a focused fashion, with attention paid to the balance between Omega-3 and Omega-6 (a group of fatty acids linked to increased inflammation). An imbalance can adversely impact well being and brain health.
8. Not all Omega 6s are bad! One known as DGLA (Dihomo-gamma-Linoleic Acid) is an antiinflammatory Omega 6 fatty acid. Other ones known as LA (Linoleic Acid) and AA (Arachindonic Acid) can be inflammatory in high amounts or when not in balanced amounts compared with DGLA. 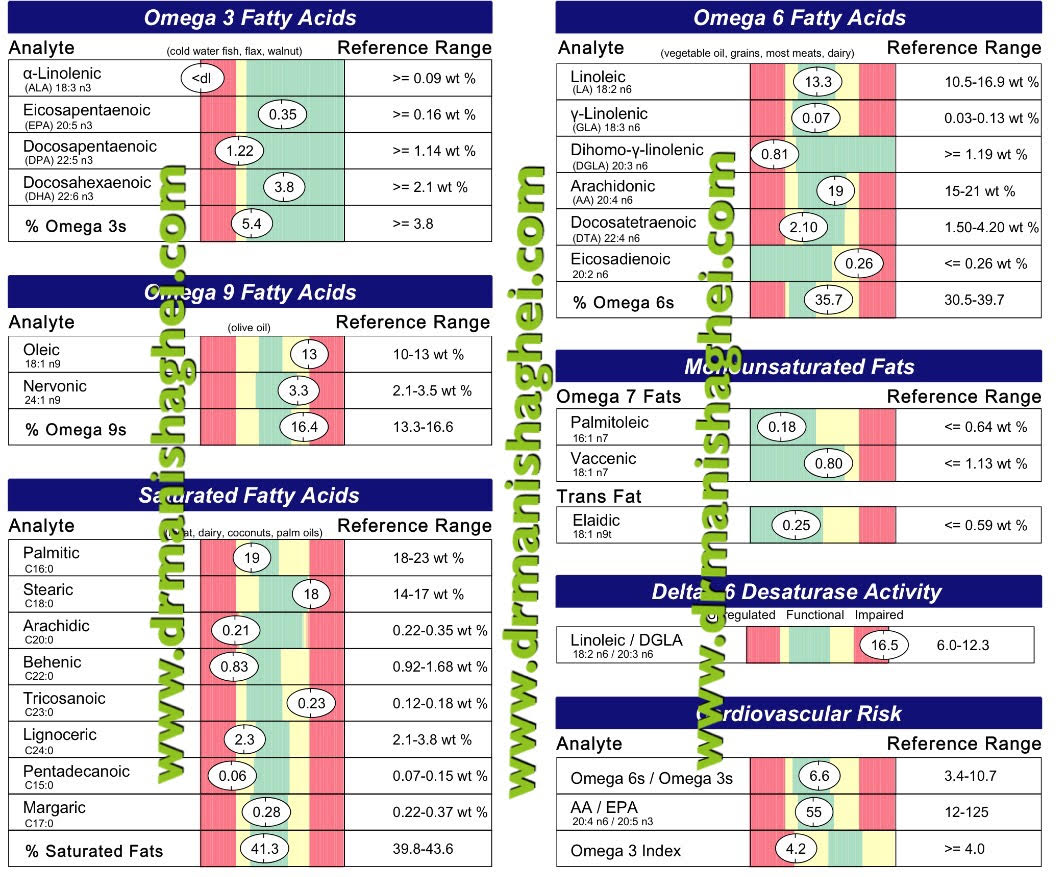
In my testing I look at individual levels of these key Omega 3 and 6 Fatty Acids but also the ratio of Linoleic to DGLA as seen in the image above. A simple blood test can give me all of the above information.
Consult your Functional Medicine and / or Integrative Holistic Medicine physician to assess your intake, test your levels, and explore ways to help you protect your health and cognitive function with essential Omegas.
References:
-
University of Maryland CAM Database Online. “Omega-3 Fatty Acids” Accessed 7 Nov 2016: http://umm.edu/health/medical/altmed/supplement/omega3-fatty-acids
-
Assisi A., Banzi R., Buonocore C., et al. “Fish oil and mental health: the role of n-3 long-chain polyunsaturated fatty acids in cognitive development and neurological disorders.” Int Clin Psychopharmacol. 2006 Nov;21(6):319-36. Accessed 7 Nov 2016: https://www.ncbi.nlm.nih.gov/pubmed/17012979
-
Ricardo U., Dangour, A.D. “Nutrition in Brain Development and Aging: Role of Essential Fatty Acids” Nutrition Reviews (May 2006)64 (suppl 2) S24-S33; DOI: 10.1111/j.1753-4887.2006.tb00242.x http://nutritionreviews.oxfordjournals.org/content/64/suppl_2/S24
-
Bourre, J.M. “Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain. Part 2: macronutrients”. J Nutr Health Aging. 2006 Sep;10(5):386-99. Accessed 7 Nov 2016: http://www.bourre.fr/pdf/publications_scientifiques/260.pdf
-
NutritionData.com. Foods Highest in Total Omega-3 Fatty Acids. Accessed 7 Nov 2016. http://nutritiondata.self.com/foods-012140000000000000000.html?maxCount=20
-
Freund-Levi Y, Eriksdotter-Jonhagen M, Cederholm T, et al. “Omega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: a randomized double-blind trial.” Arch Neurol. 2006 Oct;63(10):1402-8. Accessed 7 Nov 2016: http://www.utdallas.edu/~tres/papers/freund-levi.2006.pdf
The information offered by this blog is presented for educational purposes. Nothing contained within should be construed as nor is intended to be used for medical diagnosis or treatment. This information should not be used in place of the advice of your physician or other qualified health care provider. Always consult with your physician or other qualified health care provider before embarking on a new treatment, diet or fitness program. You should never disregard medical advice or delay in seeking it because of any information contained within this blog.
© Praana Integrative Medicine & Holistic Health Center, LLC. All rights reserved
Dr. Manisha Ghei April 16th, 2017
Posted In: Blog Post, Food, Functional Medicine, Integrative Medicine
Tags: ADHD, allergies, antioxidant, arthritis, asthma, blood pressure, cancer, cholesterol, Chronic fatigue syndrome, dementia, Diabetes Mellitus, fibromyalgia, functional medicine, healthy heart, heart healthy foods, Inflammation, Insulin, Memory, nutrition, Omega 3, vascular health
2 Comments

Interesting fact: The earliest known written record that likely referred to diabetes was in 1500 B.C in the Egyptian Ebers papyrus. It referred to the symptoms of frequent urination.
Basically, diabetes is a disease in which the body experiences elevated levels of blood sugar (glucose) due to an inability to either produce or use insulin. Most of the food we eat is turned into glucose, which our body needs for energy. In response to the rise in blood glucose, the pancreas makes a hormone called insulin, to help move the glucose into our cells for an ongoing source of energy. When you have diabetes, the body either doesn’t make enough insulin (Type-1 DM) or can’t use its own insulin efficiently (Type-2 DM). This causes glucose to build up in the blood, creating a potentially dangerous situation.
Type-1 DM is a chronic auto-immune health condition in which the immune system ravages the insulin-producing cells of the pancreas, causing a loss of the hormone insulin and affecting the way glucose is metabolized. Because of the loss of insulin, the body cannot move glucose from the blood into the cells where it is needed. Instead, glucose levels run high in the blood causing system-wide damage. While Integrative holistic health approaches can support the body, there is no cure once the pancreas are completely damaged and life-long management REQUIRES insulin. As a functional medicine doctor I have see halting of the disease process and even reversal if on early testing of the patient, the anti-bodies specific for type 1 diabetes are picked up and appropriate measures instituted. For more information on this contact my office.
Type-2 DM develops from lifestyle choices. A highly preventable disease, it was once most common in middle-aged and older people. Today, it strikes an alarming number of young adults and children. It’s directly related to poor eating and exercise habits, which typically results in being overweight – a risk factor for Type-2 DM. In this type of diabetes, your body produces insulin but does not recognize and use it properly. If health is not restored through diet, lifestyle changes, and holistic approaches, Type-2 DM can progress to a state in which insulin is required.
insulin resistance & Pre-diabetes are your warning signs, conditions, respectively in which your insulin levels are high but the body cannot utilize it appropriately and the blood glucose level is chronically above normal, but not yet high enough to be diagnosed as Type-2 DM. These stages is your chance to stop the onset of diabetes in its tracks by improving your lifestyle choices.
A few simple guidelines can help you manage diabetes, and even prevent Type-2 DM:
- Eat fresh whole foods, drink plenty of water, increase dietary fiber and the amount of dark fruits and veggies in your daily diet. Avoid processed foods and added sugars. Eat what a plant makes, not what is made in a plant!
- Exercise 30 minutes per day everyday.
- Supplement with a good high quality multivitamin/mineral, pure Omega-3 Essential Fatty Acids and B- complex vitamin with activated bioavailable forms of B vitamins.
- Test your vitamin D levels and make sure they are optimal. Take supplementation if necessary to raise levels.
- To get higher support for blood sugars try a supplement formulation specially created for that purpose and a meal replacement shake which has ingredients that support a healthy blood sugar and weight.
- Try a safe and guided detoxification protocol a few times a year especially in the spring and the fall to give a “reboot” service to your body.
- Consult with a registered dietitian with functional medicine training or a Health Coach to learn how to plan and prepare healthy meals.
- Ask your Functional medicine doctor about food allergy and sensitivity testing; nutritional deficiency testing; and comprehensive gut function testing. Also check into your adrenal health as high cortisol levels can lead to or exaggerate your condition.
- Make sure you’re not constipated. If so increase fiber in your diet, and if needed try safe supportive supplements. Daily bowel movement(s) is imperative to good health!
- Take high quality multi-species probiotic supplements in the capsule or powder forms. These come in refrigerated or shelf stable forms. I love to use the latter during my travels!
- Keep your skin healthy (hydration and whole foods). Use non-toxic personal care products
- Use natural remedies such as herbal supplements, vitamins, detoxification, and dietary adjustments under the supervision of a Board certified Integrative Medicine (ABOIM) physician and Functional Medicine trained physician (IFMCP). Try a safe and guided detoxification protocol a few times a year.
- Take medications or supplements as directed by your primary care doctor or endocrinologist.
- Take particular care of your feet. Carefully monitor wounds, because many people with DM experience poor circulation and neuropathy. Vitamin C and zinc can help support would healing
- Don’t forget to take care of your mind and spirit! Emotions, stress, lack of sleep all affect the metabolic functioning of the body. Practice mindfulness of some form daily!
If you’ve been diagnosed with Diabetes mellitus (DM), or even pre-diabetes and Insulin resistance, don’t take it lightly. Follow treatment plans and lifestyle recommendations strictly. Left untreated, diabetes can lead to many complications such as heart disease, blindness, kidney failure, and lower-extremity amputations. It’s the seventh leading cause of death in the United States.
References
-
Murray, M.T., “Diabetes Mellitus” in Pizzorno, Joseph E. (2013). Textbook of Natural Medicine. St. Louis, MO Elsevier. p. 898; 1340; (chapter 161), 1320-1348.
-
National Institutes of Health. Diabetes. https://www.niddk.nih.gov/health-information/diabetes/types
-
Joslin Diabetes Center. http://www.joslin.org/info/general_diabetes_facts_and_information.html
-
Centers for Disease Control. Rates of Diabetes Diagnosed. http://www.cdc.gov/diabetes/statistics/prev/national/figbyage.htm
-
Weston A Price Foundation: Treating Diabetes. http://www.westonaprice.org/modern-diseases/treating-diabetes-practical-advice-for-combatting-a-modern-epidemic/
Image attribution: AndreyPopov/bigstockphoto.com
The information offered by this blog is presented for educational purposes. Nothing contained within should be construed as nor is intended to be used for medical diagnosis or treatment. This information should not be used in place of the advice of your physician or other qualified health care provider. Always consult with your physician or other qualified health care provider before embarking on a new treatment, diet or fitness program. You should never disregard medical advice or delay in seeking it because of any information contained within this blog.
© Praana Integrative Medicine & Holistic Health Center, LLC. All rights reserved
Dr. Manisha Ghei February 19th, 2017
Posted In: Blog Post, Functional Medicine, Integrative Medicine, Uncategorized
Tags: Diabetes Mellitus, functional medicine, healthy heart, heart disease. heart health, heart health, heart health month, heart healthy foods, holistic medicine, Insulin, Insulin Resistance, metabolic syndrome, supplements, toxins, Type 1 diabetes
Leave a Comment

Most people have their blood pressure, heart rate, lipid profile, fasting blood sugar, and even vitamin D levels measured during their yearly physical. Your physician may do an EKG or a stress test. All of these tests may be “normal,” but there are other significant risk factors for metabolic issues that contribute to cardiovascular disease, that may be completely missed unless more testing is done.
Below is a list of some easily run lab tests and calculations which give insight into risk for insulin resistance, metabolic syndrome,
inflammation and risk for future coronary heart disease. In my opinion, these tests should most certainly be a part of any patient’s assessment for metabolic disorders and development of heart disease:
1. Triglyceride to HDL ratio
This is a
simple measure of insulin resistance, risk for diabetes mellitus type 2 and cardiovascular disease. A ratio less than 3.0 is considered normal, and more than or equal to 3.0 is suggestive of insulin resistance. An elevated ratio should prompt counseling the patient about therapeutic lifestyle change with close follow-up of metabolic markers for prevention of development of diabetes, hypertension and coronary artery disease.
2. Fasting insulin levels (and, if possible, two-hour postprandial insulin levels)
Usually at the yearly physical your physician will measure fasting blood sugar, and may even measure hemoglobin A1c levels, which are markers for pre-diabetes and diabetes. In my opinion, abnormalities in these are late developments. Insulin is a hormone produced by cells in the pancreas; it’s responsible for regulating blood sugar levels and for promoting uptake of glucose into the cells for use as energy or for storage as fat. Measuring insulin levels two hours after a glucose load may be the first indication of metabolic problems in your handling of sugar (or carbs).
Sometimes a two-hour insulin measurement may be difficult, so in my practice I measure fasting insulin levels, which are the second measure to go up. These two can be early markers of insulin resistance, much before fasting blood sugar starts going up.
Excessive insulin levels lead to increased serum triglyceride levels, decreased serum HDL (good cholesterol) levels, increase in levels of the small dense LDL (the plaque-promoting form of bad cholesterol) particles. Insulin resistance is a risk factor for hyperlipidemia, diabetes, hypertension, all of which contribute to atherosclerosis and plaque formation, which in turn is a risk factor for heart disease development. I encourage my patients to work toward a fasting insulin level of at least less than 6 microunits per mL (ideal is 4). Obviously diet is the key for reducing Insulin levels, but for patients who need additional short or long term support, I use a supplement known as
Blood Sugar Support which have all the key factors to support blood sugar and insulin levels. It has helped many of my patients.
3. High-sensitivity C-reactive protein (hsCRP)
CRP is produced in the liver in response to nonspecific inflammation in the body. The high-sensitivity CRP is
an assay which detects low levels of CRP specific to inflammation in the blood stream i.e., vascular inflammation, which could be the cause for development and progression of heart disease. Standard lipid tests do not test for inflammation, and this marker can be easily tested through your local labs. Even if your lipid profile is normal and you do not have other cardiovascular disease risk factors like hypertension or obesity or diabetes, if this marker is elevated, it is cause for concern. If somebody has already had a cardiac event like a heart attack or stroke, and this marker stays chronically elevated, it could be predictive of a high risk for future repeat heart attack or stroke. The therapeutic goal for hs-CRP is less than 0.7 mg/L, preferably as near to 0 as possible. I like to repeat this a few times to be sure it is actually staying high.
A word of caution with hs-CRP: though a marker of inflammation, it can also be a marker for infection and acute injury, so if you’ve had any recent surgery or procedure; have a respiratory, gum or other infection; or have the flu, please wait until your symptoms are resolved before testing, as this marker will be elevated due to that acute event.
4. Red blood cell magnesium levels
Red blood cell magnesium levels are the best way to assess magnesium status. Clinical signs of magnesium deficiency could be fatigue, weakness, muscle cramps, seizures, numbness and tingling in the extremities, mood and sleep issues, irregular heartbeats and also spasms in the arteries which feed the heart, contributing to heart attacks.
Magnesium supplementation may reduce the risk of coronary heart disease, so try to keep levels at the high end of the lab range, though I monitor clinically more often. The form of
magnesium I use is a very highly absorbable chelate.
5. Homocysteine levels
Homocysteine is a toxic amino acid and elevated levels
can be a risk factor for development of cardiovascular disease and stroke. Elevated homocysteine levels damage LDL cholesterol, causing its oxidation. Oxidized LDL leads to plaque formation in the coronary arteries. Homocysteine is produced as an intermediate in the metabolism of amino acids methionine and cysteine.
Activated forms of vitamin B12 and folate are needed for the conversion of homocysteine into methionine, so elevated homocysteine can be one of the indicators of deficiency in these important vitamins (remember that there are drugs like Methotrexate and acid blockers like Nexium which block the metabolism or absorption of these vitamins and may cause elevations in homocysteine levels). Serum homocysteine is great screening test for patients who are at a risk for cardiovascular disease and stroke, especially when there is a family history but no other known risk factors. Strive to keep levels around 8 micromoles/L. If elevated Homocysteine levels are due to a genetic variation in key enzymes of the methylation pathway then
supplementation will usually be required long-term with frequent (every 3 months) monitoring of levels.
6. Ferritin levels
Ferritin is an iron-containing protein produced in the liver, and signifies the stored form of iron. Ferritin can also be a marker of inflammation. Moderate elevation of ferritin may lead to a 2-3 times increased risk for development of diabetes. Though the normal range in your lab for ferritin can be from 12-150 ng/mL in women and 12-300 ng/mL in males, studies
have shown high ferritin levels increase cardiovascular risk. Lowering the iron stores to near optimal level of between 70-80ng/mL will improve outcomes in cardiovascular disease including reduced risk for heart attacks, strokes and also improve life expectancy. As a side note, I don’t think that ferritin levels less than 50ng/mL are in any way normal (even though your lab may show it in the normal range) and reasons for low iron stores must be looked into.
7. Testosterone levels (in males only — no correlation with heart disease has been found in women)
In males, testosterone deficiency
has been associated with a high risk for cardiovascular disease. In elderly males, lower free testosterone level has been shown to be associated with a high prevalence of cardiovascular disease. If your total and free testosterone levels are low, work within integrative or a functional medicine physician to find out why that is the case. Replacing testosterone may not be the only answer. Certain natural supplements like
Zinc,
Magnesium,
L-carnitine,
B vitamins especially B6 can help support Testosterone levels naturally.
Males should try to keep testosterone levels between 350-600ng/dl. Remember, more is not always better with testosterone therapy if you need it, and always seek out a physician well versed in male hormonal replacement therapies, or someone who can help guide you to support your body’s hormone production naturally!
8. Testing for chronic infections
Many pathogenic bugs have been shown to have a significant correlation with development of coronary heart disease as well as acute coronary syndromes (heart attacks). Some of
these are herpes simplex virus,
cytomegalovirus, and
H. pylori. Ask your physician to test for antibodies to these bugs through your local laboratories. Since most of your immune system is in the gut, taking a multistrain good quality
probiotic can be a great first step.
Print out and take this list to your physician to help them better evaluate your risk for heart disease, or find a
functional medicine physician who is well versed in managing and counseling patients with metabolic disorders!
The information offered by this blog is presented for educational purposes. Nothing contained within should be construed as nor is intended to be used for medical diagnosis or treatment. This information should not be used in place of the advice of your physician or other qualified health care provider. Always consult with your physician or other qualified health care provider before embarking on a new treatment, diet or fitness program. You should never disregard medical advice or delay in seeking it because of any information contained within this blog.
websol September 20th, 2015
Posted In: Blog Post
Tags: blood pressure, chronic disease, chronic infections, CMV, coronary plaque, February, ferritin, Folate, functional medicine, H. Pylori, healthy heart, heart attack, heart disease. heart health, heart health, Homocysteine, hs-CRP, HSV, Inflammation, Insulin, Magnesium, metabolic syndrome, oxidized LDL, testosterone, vitamin B12
Leave a Comment